
Not only vampires go out at night-LUPUS patients do too!
While these things are true-UV Hypersensitivity is prevalent with Systemic Lupus Erythematosus - it doesn't have to mean ISOLATION in this day & age!
With lupus, our bodies aren't just "allergic" to itself (white blood cells attacking healthy tissue by mistake causing central nervous system damage, kidney damage, skin damage including hives, solar urticaria, discoid, pemphigoid, and cutaneous porphyria rashes, lesions & vasculitis, inflammation around the heart-pericarditis, around the lungs-pleurisy, blood disorders (clotting issues and anemia), nerve damage and a myriad of other symptoms and conditions. So what do you do? You manage. You CONFORM!
I can tell you what I do-
My windows have double black-out drapes. I go out mostly at night only. After many years of neutragena helioplex 360 and 120 proof sunscreen-rashes and lupus flares anyway-I discovered the true way to be less sick is to just plain STAY INSIDE. In the dark. No UV lights, no sun at all. Is it isolating? I don't think so thanks to modern technology-but that's me-it's all in how you see it. "Housebound is no worse than earthbound it's what you make of it."
Here's some of my rashes from UV-if you had these I'm sure you'd come to the same conclusion!









That would drive ya inside-yes? LOL..And my point? It doesn't have to BE isolating or feel isolating..
The internet has given us many advances-immediate chat, visuals like skype, and the ability to find info, give info, and reach out without having to take one step outside into that debilitating sun. I can watch my son's chorus concert from bed, talk to people on the other side of the world-make appointments, talk to doctors and do relatively anything but reach out and touch someone! So isolating? No-it's the opposite for people like me!!! It's FREEING! And I'm thankful for it everyday! Even after a small TIA June 2012-I was relatively a "head in a bed" while I recouped...but I was happy and I was anything but bored or isolated! So again-Housebound is what you make of it! Is a wheelchair a good or a bad thing? Ask someone who is in one? It's a great thing! It's mobility! Just a different way-and so what!
On a personal note - I enjoy watching reality shows-specifically shows about Alaska-the last frontier. Why- I wonder? Because we LUPUS patients share something with these people-we are isolated. We are literally in the dark most of the time. Plus of course-they are exciting! There's gold miners, hunters, and people who are solely responsible for their own food and water sources-and live in the most extreme of circumstances. And they succeed. They flourish. They give us HOPE. They tell us that life is precious-and to be lived- There is a woman you might have all seen-Susan Aikens on a National Geographic show called "Life Below Zero", who owns and manages a remote fueling station near the Arctic Circle-she is alone 8 months of the year. She is the strongest, toughest woman I have ever seen. She was attacked by a bear, left for dead, sewed up her own head, hunts for food and braves temperatures so freezing- she doesn't just persevere-she flourishes. I designed the pic of Sue & Alaska to say Thank You for the Inspiration!
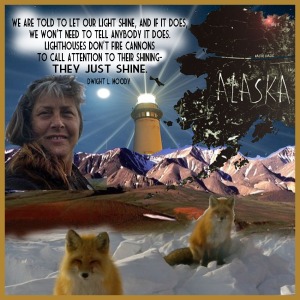
Pic of Susan Aikens from "Life Below Zero" on National Geographic channel
Susan said that she knows due to her remoteness and the difficulty especially in winter for planes and helicopters to reach her that she and people like her understand that if something happens, if they get hurt-that there is always the chance that noone will come and they will die out there. People with chronic illness know the same fear. It is freeing to accept what might happen-what could happen-it takes the fear out of it! Still-I think Susan has another message-one she might not even realize-
When Susan Aikens was asked why she is alright to stay out there in remote Alaska alone and be isolated so much of the year-she said it is because when she was little all she wanted to be was a lighthouse keeper. Well-she IS a lighthouse keeper. She's a beacon of what life without fear means for those with chronic illness. She's an inspiration.
"We are told to let our
light shine, and if it does, we won't need to tell anybody it does.
Lighthouses don't fire cannons to call attention to their shining- they
just shine"., Dwight L Moody
from Wiki on Solar Urticaria:
Solar urticaria (SU) is a rare condition in which exposure to ultraviolet or UV radiation, or sometimes even visible light, induces a case of urticaria or hives that can appear in both covered and uncovered areas of the skin.[1][2] It is classified as a type of physical urticaria.[3]
The classification of disease types is somewhat controversial. One
classification system distinguished various types of SU based on the wavelength of the radiation that causes the breakout; another classification system is based on the type of allergen that initiates a breakout.[4][5]
The agent in the human body responsible for the reaction to radiation, known as the photoallergen, has not yet been identified.[6] The disease itself can be difficult to diagnose properly because it is so similar to other dermatological disorders, such as polymorphic light eruption or PMLE.[7] The most helpful test is a diagnostic phototest, a specialized test which confirms the presence of an abnormal sunburn reaction. Once recognized, treatment of the disease commonly involves the administration of antihistamines, and desensitization treatments such as phototherapy.[1] In more extreme cases, the use of immunosuppressive drugs and even plasmapheresis may be considered.[8]
The initial discovery of the disease is credited to P. Merklen in 1904, but it did not have a name until the suggestion of "solar urticaria" was given by Duke in 1923.[6][9] However, their research contributed to the study of this uncommon disease. More than one hundred cases have been reported in the past century.[10]
The agent in the human body responsible for the reaction to radiation, known as the photoallergen, has not yet been identified.[6] The disease itself can be difficult to diagnose properly because it is so similar to other dermatological disorders, such as polymorphic light eruption or PMLE.[7] The most helpful test is a diagnostic phototest, a specialized test which confirms the presence of an abnormal sunburn reaction. Once recognized, treatment of the disease commonly involves the administration of antihistamines, and desensitization treatments such as phototherapy.[1] In more extreme cases, the use of immunosuppressive drugs and even plasmapheresis may be considered.[8]
The initial discovery of the disease is credited to P. Merklen in 1904, but it did not have a name until the suggestion of "solar urticaria" was given by Duke in 1923.[6][9] However, their research contributed to the study of this uncommon disease. More than one hundred cases have been reported in the past century.[10]
from the Lupus Foundation of America on Lupus Rashes:
Approximately
two-thirds of people with lupus will develop some type of skin disease,
called cutaneous lupus erythematosus. Skin disease in lupus can cause
rashes or sores (lesions), most of which will appear on sun-exposed
areas such as the face, ears, neck, arms, and legs.
Cancer can develop in discoid lesions that have existed for a long time. It’s important to speak with your doctor about any changes in the appearance of these lesions.
Discoid lupus lesions can be very photosensitive so preventive measures are important:
Acute cutaneous lupus lesions occur when your systemic lupus is active. The most typical form of acute cutaneous lupus is a malar rash–flattened areas of red skin on the face that resemble a sunburn. When the rash appears on both cheeks and across the bridge of the nose in the shape of a butterfly, it is known as the "butterfly rash." However, the rash can also appear on arms, legs, and body. These lesions tend to be very photosensitive. They typically do not produce scarring, although changes in skin color may occur.
Calcinosis is caused by a buildup of calcium deposits under the skin. These deposits can be painful, and may leak a white liquid. Calcinosis can develop from a reaction to steroid injections or as a result of kidney failure.
Cutaneous vasculitis lesions occur when inflammation damages the blood vessels in the skin. The lesions typically appear as small, red-purple spots and bumps on the lower legs; occasionally, larger knots (nodules) and ulcers can develop. Vasculitis lesions can also appear in the form of raised sores or as small red or purple lines or spots in the fingernail folds or on the tips of the fingers. In some cases, cutaneous vasculitis can result in significant damage to skin tissue. Areas of dead skin can appear as sores or small black spots at the ends of the fingers or around the fingernails and toes, causing gangrene (death of soft tissues due to loss of blood supply).
Hair loss can occur for other reasons besides scarring on the scalp. Severe systemic lupus may cause a temporary pattern of hair loss that is then replaced by new hair growth. A severe lupus flare can result in fragile hair that breaks easily. Such broken hairs at the edge of the scalp give a characteristic ragged appearance termed "lupus hair."
Raynaud’s phenomenon is a condition in which the blood vessels in the hands and/or feet go into spasm, causing restricted blood flow. Lupus-related Raynaud’s usually results from inflammation of nerves or blood vessels and most often happens in cold temperatures, causing the tips of the fingers or toes to turn red, white, or blue. Pain, numbness, or tingling may also occur. People with Raynaud’s phenomenon should try to avoid cold conditions, and, if necessary, should wear gloves or mittens and thick socks when in an air-conditioned area.
Livedo reticularis and palmar erythema are caused by abnormal rates of blood flow through the capillaries and small arteries. A bluish, lacelike mottling will appear beneath the skin, especially on the legs, giving a "fishnet" appearance. Like Raynaud’s phenomenon, these conditions tend to be worse in cold weather.
Mucosal ulcerations are sores in the mouth or nose or, less often, in lining of vaginal tissue. These ulcers can be caused by both cutaneous lupus and systemic lupus. It is important to differentiate lupus ulcers from herpes lesions or cold sores, which may be brought on by the use of immunosuppressive drugs. Lupus ulcers are usually painless and signs of inflammation will show up in the biopsy.
Petechiae (pah-TEE-kee-eye) are tiny red spots on the skin, especially on the lower legs, that result from low numbers of platelet in the blood, a condition called thrombocytopenia. Although thrombocytopenia is common in lupus, serious bleeding as a result of the low number of platelets usually does not occur.
A new class of drugs, called topical immunomodulators, can treat serious skin conditions without the side effects found in corticosteroids: tacrolimus ointment (Protopic®) and pimecrolimus cream (Elidel®) have been shown to suppress the activity of the immune system in the skin, including the butterfly rash, subacute cutaneous lupus, and possibly even discoid lupus lesions.
In addition, thalidomide (Thalomid®) has been increasingly accepted as a treatment for the types of lupus that affect the skin; it has been shown to greatly improve cutaneous lupus that has not responded to other treatments.
The Lupus Foundation of America would like to thank Richard Sontheimer, MD, for this information.
Medically reviewed on July 12, 2013
40-70 percent of people with lupus will find that their disease is made worse by exposure to ultraviolet (UV) rays from sunlight or artificial light.A dermatologist, a physician who specializes in caring for the skin, should treat lupus skin rashes and lesions. He or she will usually examine tissue under a microscope to determine whether a lesion or rash is due to cutaneous lupus: taking the tissue sample is called a biopsy.
The Forms of Cutaneous Lupus
Lupus skin disease can occur in one of three forms:- Chronic cutaneous (discoid) lupus
- Subacute cutaneous lupus
- Acute cutaneous lupus.
Approximately 10 percent of people with discoid lupus later develop lupus in other organ systems, but these people probably already had systemic lupus with the skin rash as the first symptom.Discoid lupus lesions are often red, scaly, and thick. Usually they do not hurt or itch. Over time, these lesions can produce scarring and skin discoloration (darkly colored and/or lightly colored areas). Discoid lesions that occur on the scalp may cause the hair to fall out. If the lesions form scars when they heal, the hair loss may be permanent.
Cancer can develop in discoid lesions that have existed for a long time. It’s important to speak with your doctor about any changes in the appearance of these lesions.
Discoid lupus lesions can be very photosensitive so preventive measures are important:
- Avoid being out in the sunlight between the hours of 10 a.m. and 4 p.m.
- Use plenty of sunscreen when you are outdoors
- Wear sun-protective clothing and broad-brimmed hats
- Limit the amount of time spent under indoor fluorescent lights
Acute cutaneous lupus lesions occur when your systemic lupus is active. The most typical form of acute cutaneous lupus is a malar rash–flattened areas of red skin on the face that resemble a sunburn. When the rash appears on both cheeks and across the bridge of the nose in the shape of a butterfly, it is known as the "butterfly rash." However, the rash can also appear on arms, legs, and body. These lesions tend to be very photosensitive. They typically do not produce scarring, although changes in skin color may occur.
Other Skin Problems
There are several other conditions that can occur with lupus:Calcinosis is caused by a buildup of calcium deposits under the skin. These deposits can be painful, and may leak a white liquid. Calcinosis can develop from a reaction to steroid injections or as a result of kidney failure.
Cutaneous vasculitis lesions occur when inflammation damages the blood vessels in the skin. The lesions typically appear as small, red-purple spots and bumps on the lower legs; occasionally, larger knots (nodules) and ulcers can develop. Vasculitis lesions can also appear in the form of raised sores or as small red or purple lines or spots in the fingernail folds or on the tips of the fingers. In some cases, cutaneous vasculitis can result in significant damage to skin tissue. Areas of dead skin can appear as sores or small black spots at the ends of the fingers or around the fingernails and toes, causing gangrene (death of soft tissues due to loss of blood supply).
Hair loss can occur for other reasons besides scarring on the scalp. Severe systemic lupus may cause a temporary pattern of hair loss that is then replaced by new hair growth. A severe lupus flare can result in fragile hair that breaks easily. Such broken hairs at the edge of the scalp give a characteristic ragged appearance termed "lupus hair."
Raynaud’s phenomenon is a condition in which the blood vessels in the hands and/or feet go into spasm, causing restricted blood flow. Lupus-related Raynaud’s usually results from inflammation of nerves or blood vessels and most often happens in cold temperatures, causing the tips of the fingers or toes to turn red, white, or blue. Pain, numbness, or tingling may also occur. People with Raynaud’s phenomenon should try to avoid cold conditions, and, if necessary, should wear gloves or mittens and thick socks when in an air-conditioned area.
Livedo reticularis and palmar erythema are caused by abnormal rates of blood flow through the capillaries and small arteries. A bluish, lacelike mottling will appear beneath the skin, especially on the legs, giving a "fishnet" appearance. Like Raynaud’s phenomenon, these conditions tend to be worse in cold weather.
Mucosal ulcerations are sores in the mouth or nose or, less often, in lining of vaginal tissue. These ulcers can be caused by both cutaneous lupus and systemic lupus. It is important to differentiate lupus ulcers from herpes lesions or cold sores, which may be brought on by the use of immunosuppressive drugs. Lupus ulcers are usually painless and signs of inflammation will show up in the biopsy.
Petechiae (pah-TEE-kee-eye) are tiny red spots on the skin, especially on the lower legs, that result from low numbers of platelet in the blood, a condition called thrombocytopenia. Although thrombocytopenia is common in lupus, serious bleeding as a result of the low number of platelets usually does not occur.
Treating Cutaneous Lupus
The medications used to treat lupus-related skin conditions depends on the form of cutaneous lupus. The most common treatments are topical ointments, such as steroid cream or gel. In some cases liquid steroids will be injected directly into the lesions.A new class of drugs, called topical immunomodulators, can treat serious skin conditions without the side effects found in corticosteroids: tacrolimus ointment (Protopic®) and pimecrolimus cream (Elidel®) have been shown to suppress the activity of the immune system in the skin, including the butterfly rash, subacute cutaneous lupus, and possibly even discoid lupus lesions.
In addition, thalidomide (Thalomid®) has been increasingly accepted as a treatment for the types of lupus that affect the skin; it has been shown to greatly improve cutaneous lupus that has not responded to other treatments.
Preventative Treatments
- Avoidance/protection from sunlight and artificial ultraviolet light
- Seek shade
- Sunscreens -- physical and chemical
Local/Topical Treatments
- Corticosteroid creams, ointments, gels, solutions, lotions, sprays, foams
- Calcineurin inhibitors
- tacrolimus ointment (Protopic®)
- pimecrolimus cream (Elidel®)
Systemic Treatments for Mild to Moderate Disease
- Corticosteroids -- short term
- Antimalarials
- hydroxychloroquine (Plaquenil®)
- chloroquine (Aralen®)
- quinacrine (available from compounding pharmacies only)
- Retinoids
- synthetic forms of vitamin A—isotretinoin (Accutane®), acitretin (Soriatane®)
- diaminodiphenylsulfone (Dapsone®)
- Sulfones
Systemic Treatments for Severe Disease
- Corticosteroids -- long term
- Gold
- oral—auronofin (Ridura®)
- intramuscular—gold sodium thiomaleate (Myochrisine®)
- Thalidomide (Thalomid®)
- Methotrexate
- Azathioprine (Imuran®)
- Mycophenolate mofetil (CellCept®)
- Biologics
- efalizumab (Raptiva®)
The Lupus Foundation of America would like to thank Richard Sontheimer, MD, for this information.
Medically reviewed on July 12, 2013
