LUPUS Neuropathies, I’ve wondered what IS the cause? Is it destruction to the myelin sheath? Is it the same as in diabetic neuropathy? Is it from inflammation in blood vessels or nerves or both?

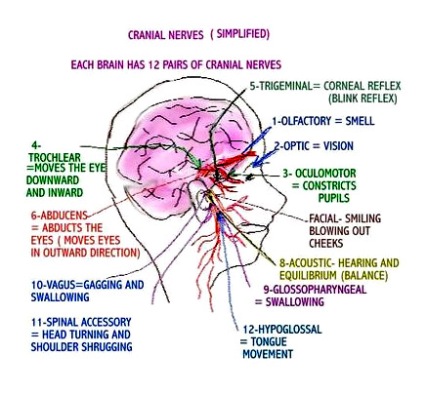
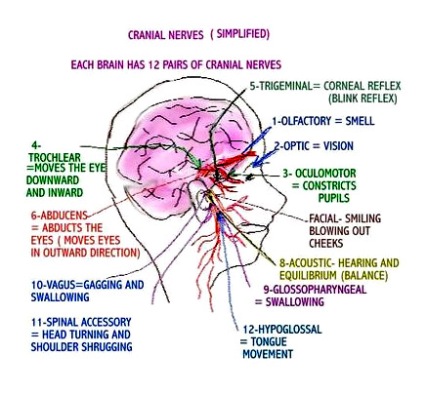
Try asking a doctor that question..lupies-ask your rheumatologists..they are not quick to “go there”, although statistics are that 20% of all patients with systemic lupus (SLE) have neuropathy and of those 20% , only 4% have cranial neuropathies. I’d be hip to hearing YOUR stories and responses from your rheumatologists on the subject, so feel free to comment!
Those statistics IMO are right on the money! I’ve met many patients with lupus online, and about a quarter of them have neuropathy and out of those in the 3 years I’ve been online hanging out in support groups, I have met just about one dozen of us with lupus and trigeminal neuralgia, geniculate neuralgia, temporal arteritis, etc. I try to share information I find on medical sites at my other site here:
http://lupuscranialneuropathies.blogspot.com/ .
Here is a good explanation of the process from Lupus International:
A variety of pathological processes may be involved in CNS lupus. The blood supply to a particular part of the brain can be disrupted due to autoimmune vasculitis (blood vessel inflammation), or clots formed as a result of antiphospholipid antibodies, or emboli that travel from a cardiac source. In some lupus patients, the thickness of their blood is increased causing hyperviscosity and this may disrupt blood flow. Anti-neuronal antibodies also may be produced in some lupus patients; these can have direct effects on the cells of the brain (neurons) and alter their function. The choroid plexus, a part of the brain that is the source of cerebrospinal fluid (CSF- a fluid bathing brain and spinal cord) may be involved thus causing diffuse problems. Several cytokines such as interleukin-1, interleukin-6 and interferon-γ are increased in CNS lupus and these have a direct effect on the neurons and can interfere with their function. Abnormalities of the hormones produced in the hypothalamus, pituitary and adrenal glands (the HPA axis) are common in lupus due to the disease itself as well as the effects of steroids and these abnormalities can cause some of the CNS disturbances lupus.
In addition, a number of secondary factors lead to the manifestations of CNS lupus such as infection (lupus patients are more prone to certain types of infections), medications (several drugs such as corticosteroids have significant CNS toxicity), hypertension, electrolyte imbalances, uremia (renal failure), thyroid disease, atherosclerotic strokes, and subdural hematomas. The concomitant presence of fibromyalgia in lupus patients is associated with an increase in functional neurological problems such as anxiety and cognitive dysfunction.
I have both peripheral and cranial (brainstem) neuropathies with myoclonic seizures. I take anti-seizure meds (tegretol) that help control them. Trigeminal neuralgia is considered to be the most painful condition known to man. There is no cure for nerve damage.
The LFA has some of the best information on lupus and neuropathy. From
http://www.lfa.org:
The Nervous System
Lupus is an autoimmune disease that can affect almost any part of your body, including your joints, skin, kidneys, heart, lungs, or blood. Lupus can also affect the nervous system and brain. There are several terms doctors use to describe this: neuropsychiatric lupus (NP-SLE), neurocognitive dysfunction, or central nervous system lupus (CNS lupus). Your nervous system has three parts, any of which may be affected by lupus.
The central nervous system (CNS) consists of the brain and the spinal cord.
The peripheral nervous system (PNS) is a network of nerves that connects the brain and spinal cord to the rest of the body, and gives skin and muscles the signals needed for sensation and movement.
The autonomic nervous system (ANS) allows communication between spinal and peripheral nerves and the brain and internal organs, and controls functions like breathing, blood flow, and heart rate.
People with lupus can experience a number of complications when their nervous system is affected. The symptoms may come on suddenly or may come and go, but they will vary depending upon the location and extent of the tissue injury. These symptoms also can be present in other diseases, so diagnosing lupus-related nervous system disorders is often difficult.
Neurologists are the physicians who specialize in the nervous system. They may rely on a number of diagnostic tools to determine whether lupus is involved in your cognitive problems:
x-rays
brain scans (magnetic resonance imaging (MRI) and computed tomography (CT)
electroencephalograms (to capture the electrical pattern of brain activity)
spinal tap (to examine fluid in the spinal column)
Behavioral and cognitive tests may also be done to find out if your memory or other mental abilities have been affected.
Depending on the symptoms, a variety of medications are available to treat lupus-related nervous system disorders, including non-steroidal anti-inflammatory drugs, antimalarials, and steroids. Your response to treatment may be rapid or gradual over several months. For many people with lupus, nervous system involvement is completely reversible.
Central Nervous System (CNS)
When lupus affects your central nervous system, many symptoms may occur, including:
headaches
confusion
fatigue
depression
seizures
strokes
vision problems
mood swings
difficulty concentrating
Drugs used to treat lupus can cause side effects that are similar to the symptoms of CNS lupus. If you have symptoms of CNS lupus you should consult a neurologist who can determine which symptoms are side effects of medication and which are due to lupus. The drugs most known for causing symptoms like those of CNS lupus are:
Non-steroidal anti-inflammatory drugs (NSAIDs) – may cause headache, dizziness, confusion, and in rare instances, meningitis-like symptoms
Antimalarials – in very high doses (not usually given for lupus) may cause manic behavior, seizures, psychosis
Corticosteroids – may cause agitation, confusion, mood swings, psychosis, depression
Anti-hypertensive medications – may cause depression or loss of sex drive
A serious form of lupus called CNS vasculitis may occur when there is inflammation of the blood vessels of the brain. Characterized by high fevers, seizures, psychosis, and meningitis-like stiffness of the neck, CNS vasculitis is the most dangerous form of lupus involving the nervous system and usually requires hospitalization and high doses of corticosteroids to suppress the inflammation.
Peripheral Nervous System (PNS)
The nerves of your peripheral nervous system control your motor responses and sensation, so symptoms of numbness or tingling, or inability to move a part of your body, may be the result of lupus affecting these nerves. Known as peripheral neuropathies, symptoms of PNS nerve damage are caused by inflammation of the nerves or by compression of the nerves due to swelling in the tissue around them. The types of symptoms you might experience include:
vision problems
facial pain
ringing in the ears
dizziness
drooping of an eyelid
carpel tunnel syndrome
Autonomic Nervous System (ANS)
The autonomic nervous system regulates many of your body’s functions that happen almost automatically: heart rate, blood pressure, feeling hot or cold, bladder and bowel functions, release of adrenalin, breathing, sweating, and muscle movement. Lupus can cause these nerve signals to be overactive, which can lead to a wide range of symptoms:
numbness
burning
tingling
mental confusion
headaches
gastrointestinal problems such as nausea, vomiting, constipation, or diarrhea
Raynaud’s phenomenon
Raynaud’s phenomenon is a condition of ANS involvement caused by inflammation of nerves or blood vessels. Blood vessels in your hands and feet go into spasm and restrict blood flow, usually as a reaction to cold temperatures, with the tips of the fingers or toes turning red, white, or blue. Raynaud’s can also cause pain, numbness, or tingling in fingers and/or toes. People who have Raynaud’s phenomenon are advised to avoid cold conditions when possible, and may have to wear gloves or mittens when in air-conditioned surroundings.
Livedo reticularis and palmar erythema are two other skin disorders that may affect you if you have autonomic nerve damage. Both of these conditions can cause a bluish, lacelike mottling under your skin, especially on your legs, giving your skin a “fishnet” look.
Cognitive Dysfunction
As many as half of all people with lupus describe feelings of confusion, fatigue, memory loss, and difficulty expressing their thoughts. This collection of symptoms is termed cognitive dysfunction, although many people call it “lupus fog.”
Cognitive dysfunction most often affects people with mild to moderately active lupus. The causes of these symptoms, and the reasons that the symptoms tend to come and go, are not known. Living with cognitive dysfunction can be very frustrating. However, you can learn to improve your concentration and lessen confusion and memory loss with a variety of coping skills, including puzzles, games, biofeedback, using a daily appointment calendar, and balancing daily activities to reduce stress.
Lupus Headache
Compared with the general population, people with lupus may be twice as likely to experience migraine-like lupus headaches, commonly known as lupus headaches. The features of lupus headaches are similar to migraines and may be seen more often in people who also have Raynaud’s phenomenon. However, headaches can also be caused by vasculitis, a symptom of active lupus due to inflammation of the blood vessels. If you are experiencing headaches that are not improved by an over-the-counter headache medication, be sure to tell your doctor.